Increasingly, considerations for talent management strategies in 2022 — and beyond — revolve around the employee experience. Employers are also showing greater interest in a formalized process for gathering workforce feedback. And this interest suggests they recognize that combining insights from different sources provides the advantage of a holistic perspective. Conducting surveys or forming committees that explore what employees value most in their benefits, perks and work culture guides better decisions and investment outcomes. For specific concerns, digging deeper into data may identify risk factors that merit a closer look.
The more effectively employers communicate their entire suite of offerings the more fully they'll engage their workforce. Twenty-seven percent (27%) agree their benefits strategy helps remote workers engage in the organization's culture, a continuing challenge exacerbated by the large-scale shift to telecommuting.3
Curating a lineup of vendors that offer holistic, personalized support
The emergence of highly targeted point solutions is a response to broad-brush population health programs, which have low engagement and limited effectiveness. These resources provide support in a narrow category such as diabetes, oncology management, behavioral health or virtual primary care.
For some categories, such as cancer, geographic location once restricted care availability. But emerging technology and telehealth solutions now allow program members and their providers to access highly specialized services across the country. Qualified healthcare professionals can weigh in on everything from the diagnosis to the treatment plan. Realizing that results are only possible if employees participate, vendors offer a digital, user-friendly front-end experience, engaging with people using familiar channels such as text messaging and apps.
With so many vendors and products popping up, a thorough evaluation and comparison of point solutions requires employers to identify gaps in their capabilities. Because these vendors tend to have a short history, establishing metrics for tracking results and then holding them accountable is critical. Ensuring that vendors complement and integrate with each other is part of a well-curated approach.
Reexamining benefits and policies through the lens of diversity, equity and inclusion (DEI)
As employers seek to align benefits more closely with employee values, DEI is a fitting opportunity. Fifty-five percent (55%) agree their organization's benefits strategy adequately addresses equity and inclusion for all employees, up from 50% in the spring of 2021.3, 4 Perceptions of organizations among the workforce are increasingly shaped by the presence, extent and quality of DEI policies, practices and programs. When evaluating current choices and future objectives through a more inclusive lens, the goal is to assess how well the people strategy supports them — and to help ensure equity.
Healthcare policies can offer examples of DEI measures that employers are taking. For instance, many offer a fertility or family planning benefit. However, underlying policies may not provide equal support for all types of families, unintentionally hurting an organization's progress toward meeting its DEI objectives. Even changing "fertility/infertility benefits" to "family planning" promotes inclusion. Employers are also more clearly defining the qualifications of same sex couples by applying parent and caregiver eligibility to leave policies and extending benefits plan participation to domestic partners.
Relatedly, transgender benefits will likely become more widely available. Gender reassignment surgery was covered by 23% of employers in 2021 and another 17% are expected to do so by 2023. The same survey shows the availability of transgender-inclusive benefits doubling within this period.5 Earning a top score on the Corporate Equality Index (CEI) and the title of "Best Place to Work for LGBTQ+ Equality," requires organizations to offer transgender benefits. This distinction can promote recruiting and retention, which may be a factor in driving adoption. The number of major U.S. employers affording transgender-inclusive healthcare coverage rose from 49 in the 2009 CEI to 949 in the 2020 CEI.6 To help ensure compliant transgender benefits, applicable state laws should be considered.
Investing in multifaceted mental health support to promote and help ensure access to care
The need to confront widespread isolation and anxiety in recent years has normalized behavioral, social and emotional health support for employers, and the employees who now let them into their lives more readily. Combined with the destigmatization of mental health issues, these relaxed boundaries have loosened the reigns on resource investments.
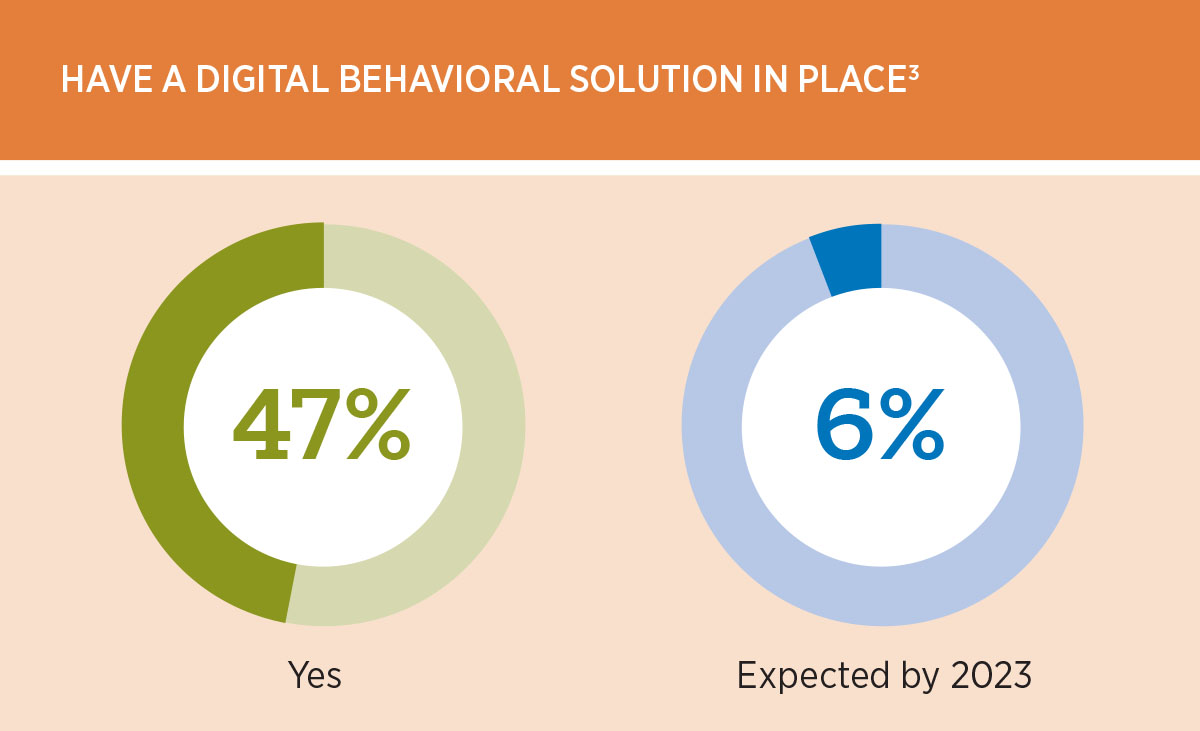
Across the board, more employers offer not only employee assistance program (EAP) services, but also resources like tele-behavioral health, targeted mobile apps, leadership training and mental health days to relieve burnout. Digital behavioral health solutions are either already in place for 47%, or are expected by 6% no later than 2023.3
With a national shortage of mental healthcare providers leading to long wait times or no availabilities, care access has moved to the forefront of concerns for many employers. Coordinating EAP services with other behavioral health point solutions, which take effect once an employee's initial included visits run out, can help fill this unmet need. It's also important to check the number of available providers that currently accept new patients to get a better sense of the benefit's actual value.
Enhancing virtual care to help ensure employees get the overall care they need
The pandemic accelerated the expansion of virtual care beyond acute medical needs, with telehealth services now available for primary care, chronic condition management and behavioral health. As employers look to extend care access — allowing them to meet employees where they are — there's interest in the opportunity to integrate virtual preventive care into the virtual primary care physician relationship.
In-person medical visits have largely resumed, prompting employers to evaluate the most effective channels for keeping health plan participants involved in their care and outcomes. Also, with a view into the appropriate mix of onsite and virtual care, point solution vendors can help guide decisions. Forty-eight percent (48%) of employers have engaged a traditional telehealth provider outside of the medical carrier, and 11% have targeted one or more specific conditions by working with a specialty vendor.3
Recent years ushered in emerging employee benefit trends, including flexibility, choice and customization that enable better work-life balance. With an eye on the future, leaders are more aware than ever of the critical role that benefits play and recognize that modernization is paramount for recruitment and retention success. Proactively exploring diverse ideas and solutions, touching base with employees on their values and priorities, and holding vendors accountable better prepares organizations to face the magnitude of challenges that change inevitably brings.